Morriston team becomes UK leader for open-heart surgery patient safety

A checklist created by cardiac staff in Morriston has seen the hospital become a UK leader in the safety of patients having open-heart surgery.
Fewer patients there now have to be taken back to theatre because of post-operative bleeding than anywhere else in the country.
See end of release for caption for main photo above
It’s down to a national award-winning checklist the cardiac surgical team developed to identify and correct all possible causes of bleeding before the chest is closed.
The benefits are huge, not only in terms of patient outcomes but also in the use of precious NHS resources. It also means fewer planned operations have to be cancelled, and has led to improved staff morale.
Post-operative bleeding is a common but major complication after open-heart surgery. From previous work in the cardiac surgical unit, the causes for return to theatre for excessive post-operative bleeding were identified.
 The source of bleeding could be surgical, requiring further suturing, or just as commonly due to problems with deranged coagulation – a condition that prevents formation of blood clots.
The source of bleeding could be surgical, requiring further suturing, or just as commonly due to problems with deranged coagulation – a condition that prevents formation of blood clots.
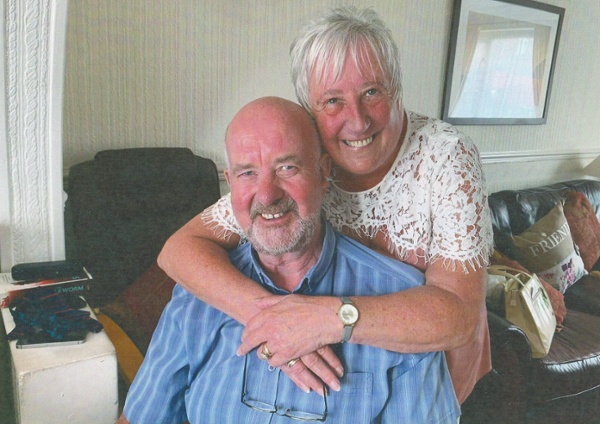
Right: Dave Bostock, pictured with wife Marilyn, underwent open-heart surgery at Morriston Hospital one year ago. He described the standard of care as superlative
Cardiothoracic consultant surgeon Pankaj Kumar said: “There is a return to theatre rate in every cardiac centre in the UK and indeed the world over.
“Over seven or eight years, our return to theatre rate was just over four per cent. A range of two to eight percent is recorded nationally and internationally, so ours sat in the middle of the pack.”
Mr Kumar said various checklists were used around the world but they were not universal. So the cardiac surgical team designed their own.
All the team had an input in its creation, and the entire team also runs through the checklist, covering off all potential surgical and coagulative causes of bleeding.
Only then is the patient’s chest closed at the end of the operation.
The list was introduced for all open-heart surgery in August 2021, and the outcomes of cases before and after have now been compared.
“Some surgeons introduced it before last August in a limited manner, which brought our return to theatre rate down to two per cent,” said Mr Kumar.
“But since August it has dropped to 0.7 per cent. That is the lowest rate in the UK now, by a considerable margin.
“The entire team has worked very hard to achieve this positive outcome for patients undergoing open-heart surgery in our unit. The challenge is to hold it there. If we can achieve that, we will be delighted.”
Someone who is already delighted is 69-year-old Dave Bostock, one of the hundreds of patients to have successfully undergone open-heart surgery since the checklist was introduced.
In fact, it’s almost exactly one year since Mr Bostock, from Llangynwyd, near Maesteg, was operated on by Mr Kumar.
“I had finished my working life but got bored and began doing some work as a caretaker in a large comprehensive school,” he said. “I was walking 26,000-27,00 steps every day.
“Then I started coughing up blood.”
 Mr Bostock underwent various tests before it was finally discovered the mitral valve in his heart had split. “My blood wasn’t being pumped around my body properly.”
Mr Bostock underwent various tests before it was finally discovered the mitral valve in his heart had split. “My blood wasn’t being pumped around my body properly.”
He was referred to Mr Kumar, who saw him in August 2021. Surgery took place on December 8th last year.
“I had no problems at all. They took me down to theatre at 8.15am and woke me up at 4.30pm. At 4.45pm, I was sitting up, having a drink. I was talking to my wife at 7pm. I was sitting up in bed, quite happy.”
A year on, Mr Bostock is doing well. Although he cannot walk as fast as he used to, he no longer gets out of breath. And he has nothing but praise for the Cardiac Centre’s staff.
“The standard of care was superlative,” he said. “I can’t fault it.”
Morriston Hospital’s award-winning cardiac surgical team
And while there are clear benefits for patients, there are also positive consequences for the wider NHS.
One of the most important of these is a reduction in the use of blood products; red cells, fresh frozen plasma and platelets – down by 66 per cent, 74 per cent and 37 per cent respectively.
Reduction in the use of these blood products alone is on target for a saving of around £120,000 over a year’s clinical activity.
There are other financial gains. Patients recover quicker, so do not have to spend as much time in the Cardiac Centre’s intensive care unit.
“One patient per bed costs around £1,600 a day in the critical care area,” said Senior Clinical Fellow Sobaran Sharma, who led the checklist project. “So the length of stay can make a big difference from that perspective.
“Also, when patients have to go to theatre a second time, other surgery due to have taken place has to be postponed.
“The patients and relatives affected are then upset. So there is the human factor, as well as the cost of the session being lost.”
This human factor applies to staff too.
Having to be called out, often during the early hours, for these emergency cases needing to go back to theatre for bleeding inevitably has an impact on the team’s morale and well-being.
Scrub nurse Victoria Jobson said working through the checklist did not take up any more time but made a massive difference.
She said: “There are only a limited number of us. If we’ve been in all night then obviously we’re not going to be in the next day and, as Mr Sharma said, cases are postponed to another time and that costs money.
“The checklist has stopped us being called in all the time. It has improved our well-being and obviously the patient’s well-being. From the department’s point of view, it has made a big impact.”
Senior clinical perfusionist Ian Bennett echoed those sentiments.
“In terms of our morale and well-being, it’s not great coming back at four in the morning. But for the patient there is an increased risk if they have to come back to theatre,” he said.
“We want to get it right first time and this is what we strive to do. Sometimes we still have to bring patients back but the list has helped.
“Looking at the wider picture, from the business angle as well, there are great savings to be made and that is obviously important.
“But from a patient’s point of view, if this stops the patient coming back to theatre, it’s job done for us.”
 Cardiac registrar Sam Poon agreed that the list had not only helped with morale but with confidence too.
Cardiac registrar Sam Poon agreed that the list had not only helped with morale but with confidence too.
“A checklist, especially when you are having a long, tiring day, does help because tired surgeons are prone to making mistakes,” he said.
“When a trainee is closing a chest and then coming back to theatre, it does have some impact on confidence level as well.
“If the re-exploration rate is persistently high, you question your chest-closing ability and that impacts on confidence.
“Since the checklist was implemented, I can’t remember the last time I was in theatre for re-opening. So this is a positive.”
The team has since gone on to win at this year’s NHS Wales Awards, in the Improving Patient Safety category (pictured right).
Mr Kumar, who is also Morriston’s Deputy Medical Director, said the entire cardiac surgical team had been delighted to receive the award.
“We feel the collective effort from the whole team has resulted in a significant improvement in a very important patient safety and quality matrix after open heart surgery.
“Patients having heart surgery here can be reassured the entire team is continuously working together to improve outcomes for them.”
Main photo top of page shows: Front row (l-r) cardiac theatre scrub staff Chito Fababeir and Victoria Jobson, and Sobaran Sharma, senior clinical fellow, cardiothoracic surgery. Back row (l-r) Mark Vernon, trainee clinical perfusionist, Ian Bennett, senior clinical perfusionist, Pankaj Kumar, consultant cardiothoracic surgeon and Deputy Medical Director, Morriston Hospital.
Rydym yn croesawu gohebiaeth a galwadau ffôn yn y Gymraeg neu'r Saesneg. Atebir gohebiaeth Gymraeg yn y Gymraeg, ac ni fydd hyn yn arwain at oedi. Mae’r dudalen hon ar gael yn Gymraeg drwy bwyso’r botwm ar y dde ar frig y dudalen.
We welcome correspondence and telephone calls in Welsh or English. Welsh language correspondence will be replied to in Welsh, and this will not lead to a delay. This page is available in Welsh by clicking ‘Cymraeg’ at the top right of this page.