De Quervains Tenosynovitis
To view this document as a pdf; click here
What is De Quervain’s Disease?
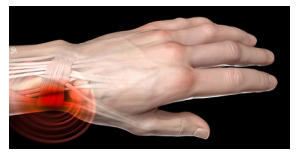
De Quervain’s Disease is a painful condition that affects the tendons located on the thumb side of your wrist. These tendons run in a tunnel (tendon sheath). Thickening of the ligamentous structure over this tunnel can cause pain when the thumb is moved or used.
What causes De Quervain’s Disease?
In most patients it occurs for no apparent reason. Occasionally it can occur following minor injury, from overusing your thumb or wrist or in young mothers, from picking up their baby. It is more common in women than men.
What are the symptoms?
Symptoms may include pain when you move your wrist or thumb and swelling or soreness on the thumb side of your wrist.
How is De Quervain’s Disease diagnosed?
It can usually be diagnosed on examination. Occasionally, x-ray or ultrasound may be required to exclude other conditions, which may mimic the symptoms of De Quervain’s Disease.
What treatments are available to treat De Quervain’s?
1. Self-Management Strategies
A) Supports/Braces
If the symptoms are mild and recent, then a splint or brace to rest the thumb and wrist may help. The pictures below show the type of support which can help. Your local Pharmacist may supply a range of supports, or you may choose to order online.
The support can be used during daily tasks, but only for short periods of time to prevent muscles from weakening. It can be worn at night if it allows you to sleep better. It may need to be worn for at least 3 weeks, to allow for any swelling to settle.

B) Modify Activities
Activities that make your symptoms worse may need to be avoided or modified whilst your thumb/ wrist recovers
C) Ice
Ice can help reduce pain and swelling. However, do not use if you have sensitivity to cold/numbness in the area or high blood pressure. When using ice never apply directly onto the skin surface as this may result in an ice burn.
Always ensure that ice is wrapped in a damp cloth to prevent a burn. Leave the ice pack in place for 15 minutes to achieve the desired effect to the area. Apply ice packs every 2 hours to the affected area of the skin in the initial couple of days.
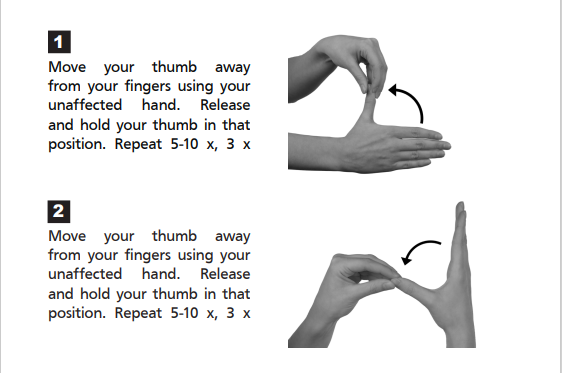
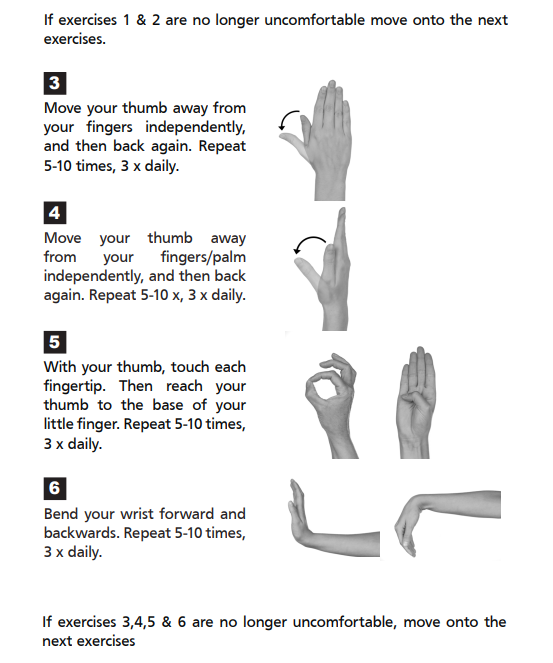
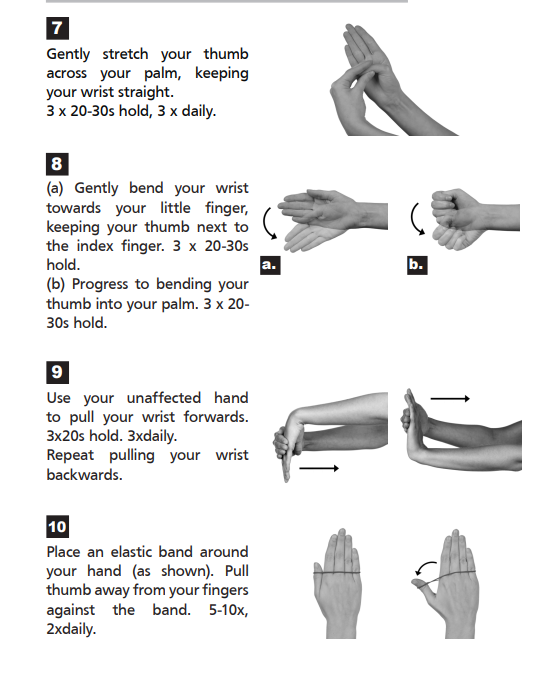
D) Exercises
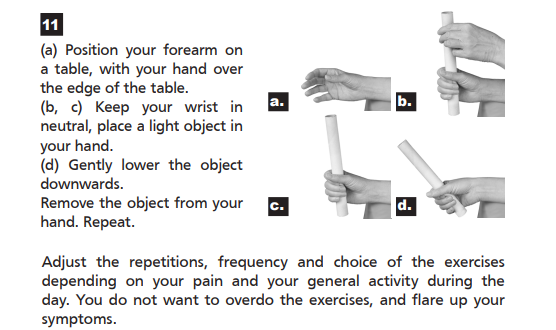
If your symptoms settle, then stretching and strengthening exercises may help to increase your hand function. e.g.
E) Kinesiotaping
This can be used to reduce pain, reduce swelling, assist movement and provide support, depending on how it is applied. The tape is applied to clean, dry, preferably hair-free skin at varying angles and at varying degrees of stretch, depending on what is being treated. There are many different taping techniques shown online and you may need to try several to see which works best for you.
Some suggestions can be found at the bottom of this page.
F) Medication
Non-steroidal anti- inflammatory medication (NSAIDs) or gels such as ibuprofen may be beneficial. You may need to discuss with your GP or pharmacist to check you are suitable to take them. A combination of the above treatments is more effective, than each one on its own.
2. Other Treatments that your Doctor may recommend
If the self-management approach does not help your symptoms and you find that your everyday activity is still being affected, then you may need to contact your GP. The following treatments may be considered;
A) Electrotherapy or acupuncture.
You will need to be referred to Physiotherapy for this.
B) Steroid Injection
A steroid injection may be of benefit if the symptoms persist or recur. A corticosteroid injection combined with anaesthetic may help to reduce the pain and swelling. The steroid is injected into the tendon sheath.
There are very small risks involved with an injection including infection, tendon weakness, or lightening of the skin. It may take some time for the injection to work. Further injections may be considered but generally may be less effective than the first.
C) Surgery
In more severe cases and if conservative treatments have failed, then surgery may be recommended. This can be performed as a day case which means you can go home the same day as your operation. This is usually done under a local anaesthetic, meaning you are not put to sleep.
The operation involves dividing part of the roof of the tendon sheath in which the tendons run. This allows the tendon to move more freely, relieving the inflammation and the pain. Your hand may be placed in a bulky dressing or plaster for 10-14 days until the wound has healed. You may be referred to see a Physiotherapist. It is advisable to avoid heavy manual work for 4-6 weeks after the surgery.
Further information on the procedure and after care will be provided by your specialist if this is the option of choice.
Rydym yn croesawu gohebiaeth a galwadau ffôn yn y Gymraeg neu'r Saesneg. Atebir gohebiaeth Gymraeg yn y Gymraeg, ac ni fydd hyn yn arwain at oedi. Mae’r dudalen hon ar gael yn Gymraeg drwy bwyso’r botwm ar y dde ar frig y dudalen.
We welcome correspondence and telephone calls in Welsh or English. Welsh language correspondence will be replied to in Welsh, and this will not lead to a delay. This page is available in Welsh by clicking ‘Cymraeg’ at the top right of this page.